Ministry of Health Presents Data on Federal Medical Center Quality Oversight
In an effort to shed light on the ongoing debate between medical insurers and the Mandatory Medical Insurance (OMI) system regarding oversight of healthcare quality, the Ministry of Health has provided «Kommersant» with data concerning the transfer of this control in federal medical centers to the OMI Fund in 2021. While the Ministry itself states that the quality of services in these centers has not declined, insurers and patient advocacy groups observe a significant reduction in investigations and expert involvement under the OMI Fund`s supervision. Meanwhile, patients continue to lodge complaints with insurers, with approximately 70% of these claims proving justified. Citing its interpretation, the Ministry aims to empower regions to reject medical insurance services, a move that insurers warn could leave patients without adequate protection.
The Ministry of Health shared statistics with «Kommersant» concerning the quality control of medical assistance in federal hospitals and clinics since 2021. This was the year when this oversight responsibility was transferred from medical insurance organizations to the Federal Mandatory Medical Insurance Fund (FFOMS), which is also responsible for financing this assistance. The request for this information was prompted by reports from the Accounts Chamber, which assessed FFOMS`s budget execution for 2022–2024. These reports indicated that insured persons` complaints were not reviewed, and expert examinations were not conducted during this period.
Conversely, the Ministry claims that between 2021 and 2025, the fund conducted 186,000 medico-economic examinations and 68,000 medical care quality examinations (MCQE), with a strong emphasis on the latter. This surge is evident in the substantial increase in MCQE, from 2,400 cases in 2021 to 21,000 in 2024. The Ministry further clarified that by 2025, 17,500 examinations, including multidisciplinary ones, had already been completed. Each year, FFOMS approves a schedule for planned quality examinations targeting high-demand medical areas, such as IVF, anti-cancer therapy for oncological diseases, and medical rehabilitation.
For 2025, planned MCQEs were arranged for 955 specific cases. Additionally, the fund plans to evaluate the quality of care for diabetes and blood disorders by the end of the year.
The Ministry underscored that the fund`s unified registry of experts currently includes over 9,000 specialists, with 192 of them engaged in assessing medical procedures in 2025. The Ministry interprets this data as evidence that the quality of treatment in federal medical institutions remains high, suggesting that this quality control model could be expanded to include regional and municipal hospitals. Consequently, when submitting the draft budget for the OMI system for 2026–2028 to the State Duma, the Ministry proposed granting regions the right to transfer insurer functions to territorial OMI funds.
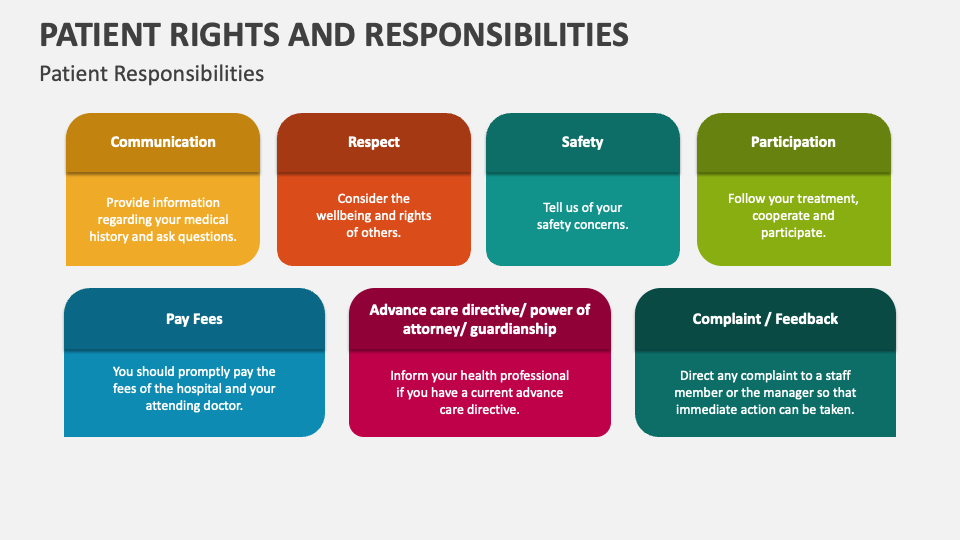
It is important to recall that insurers within the OMI system are mandated to safeguard patients` interests against state hospitals and clinics. Their responsibilities include reviewing documentation, evaluating the correctness of treatment, and informing insured individuals about preventative measures and available programs. Furthermore, they possess the authority to impose fines on medical institutions and retain a portion of the allocated funds for administrative expenses. In 2020, the State Duma initiated a move to remove medical insurers from the quality control of high-tech medical care (HTMC) in federal medical organizations. This measure was intended to generate savings that could then be redirected towards implementing OMI medical services in various regions; the functions of HTMC expertise were subsequently transferred to FFOMS. Annually, FFOMS allocates between 40 and 65 billion rubles for HTMC in federal medical centers, which facilitates approximately 200,000 hospitalizations.
However, Roman Shcheglevatykh, Vice-President of the All-Russian Union of Insurers for Medical Insurance, contends that despite the transfer of medical care payment and examination functions in federal organizations to FFOMS, patients consistently continue to seek assistance and protection from insurers.
«The figures are substantial; insurance companies receive around 1,500 inquiries per month concerning care provided in federal medical institutions,» he noted. «It`s also crucial to highlight that when reviewing patient complaints, insurers frequently side with the patients. Approximately 70–75% of all complaints are deemed justified, which clearly demonstrates insurers` vested interest in protecting patient rights.»
Why the Government Proposes Transferring Insurers` Powers in Regions to OMI Funds
Yury Zhulev, Co-Chairman of the All-Russian Union of Patients, points out another vital function performed by insurers: «Insurance representatives helped people navigate the healthcare system, explained the procedures for receiving care, and protected their rights when problems arose. Medical insurers have a well-established infrastructure for this—including call centers, hotlines, digital feedback services, and effective SMS notification systems. Territorial OMI funds currently lack such extensive infrastructure, and if the institution of insurance representatives is abolished, patients will face significantly greater challenges in obtaining support and resolving any emerging issues.»